Introduction
Dealing with an infected tooth can be painful and uncomfortable. When an infection becomes severe, tooth removal is often recommended to prevent the spread of bacteria to other parts of the mouth and body. This guide will cover everything you need to know about infected tooth removal, from recognizing the symptoms of an infection to understanding the removal process and recovery tips.
What Causes a Tooth Infection?
A tooth infection, also known as a dental abscess, occurs when bacteria invade the tooth’s inner structure or surrounding gum tissue. Common causes include:
Deep Cavities: Untreated cavities can reach the pulp, the tooth’s inner tissue, causing infection.
Gum Disease: Advanced gum disease can lead to pockets that harbor bacteria around the tooth.
Injury or Trauma: Cracked or chipped teeth can allow bacteria to reach deeper layers.
Poor Dental Hygiene: Inadequate brushing and flossing can lead to plaque buildup, causing decay and infection.
An infected tooth needs immediate attention to prevent the infection from spreading, potentially leading to more severe health problems.
Signs and Symptoms of a Tooth Infection
Recognizing the signs of an infected tooth early can help you get the treatment you need before complications arise. Common symptoms include:
Intense Toothache: Persistent pain is often the first sign of an infection.
Swelling and Redness: Swollen gums around the infected tooth and redness can indicate an infection.
Bad Taste in the Mouth: Pus from the infection can cause an unpleasant taste.
Fever and Fatigue: In more severe cases, the infection may cause fever and general tiredness.
Sensitivity to Hot or Cold: Infected teeth are often sensitive to temperature changes.
If you experience any of these symptoms, it’s essential to see a dentist promptly for a diagnosis and treatment.
When is Infected Tooth Removal Necessary?
Infected tooth removal is usually a last resort, only performed when other treatments are ineffective. Removal may be necessary if:
The Infection is Severe: If the infection has spread to surrounding tissues or cannot be treated with antibiotics or a root canal.
Iframe sync
The Tooth is Badly Damaged: When decay or damage is extensive, and saving the tooth is impossible.
The Infection Threatens Health: In some cases, untreated tooth infections can lead to other health problems, including bone loss in the jaw or infections in other parts of the body.
Your dentist will evaluate the extent of the infection and discuss the best options with you, including whether removal is needed.
The Infected Tooth Removal Process
Examination and Diagnosis
Before removing an infected tooth, the dentist will thoroughly examine the area, which may include X-rays. The X-ray helps the dentist assess the tooth’s roots and surrounding bone to determine the best course of action.
Local Anesthesia
To make the process as comfortable as possible, the dentist will administer local anesthesia to numb the area around the infected tooth. For patients with dental anxiety, sedation options may also be available.
Extraction Procedure
The extraction process depends on the tooth’s position and the severity of the infection. There are two types of extractions:
Simple Extraction: If the infected tooth is visible and easily accessible, the dentist will use a tool called an elevator to loosen it, followed by forceps to remove it.
Surgical Extraction: For more complex cases, such as impacted or broken teeth, a minor surgical procedure may be needed. This process involves making an incision in the gum to access the tooth and remove it.
Cleaning the Area
Once the tooth is removed, the dentist will thoroughly clean the area to ensure no infection remains. In some cases, the socket may be stitched closed to aid in healing.
Post-Extraction Instructions
The dentist will provide instructions on caring for the extraction site, which may include tips on managing pain, cleaning the area, and dietary recommendations.
Aftercare Tips for Infected Tooth Removal
Proper aftercare is essential for a smooth recovery and to prevent complications after infected tooth removal. Here’s what to keep in mind:
Manage Pain and Swelling: Use prescribed pain relievers and apply an ice pack to the outside of the cheek to reduce swelling.
Avoid Certain Foods: Stick to soft foods and avoid hot, spicy, or crunchy items that could irritate the site.
Keep the Area Clean: Gently rinse your mouth with a saltwater solution after 24 hours, but avoid vigorous rinsing or spitting to prevent dislodging the blood clot.
Rest and Avoid Physical Activity: Take it easy for a few days and avoid strenuous activities that could increase blood flow to the area.
Do Not Smoke or Use a Straw: Smoking and using straws can cause dry socket, a painful condition where the blood clot dislodges from the extraction site.
Following these aftercare instructions can help prevent infection and ensure proper healing.
Possible Complications After Tooth Removal
While most extractions heal without complications, it’s essential to watch for any signs of problems. Contact your dentist if you experience:
Excessive Bleeding: Light bleeding is normal, but excessive bleeding is a sign of concern.
Prolonged Pain and Swelling: Pain and swelling that doesn’t improve after a few days may indicate infection.
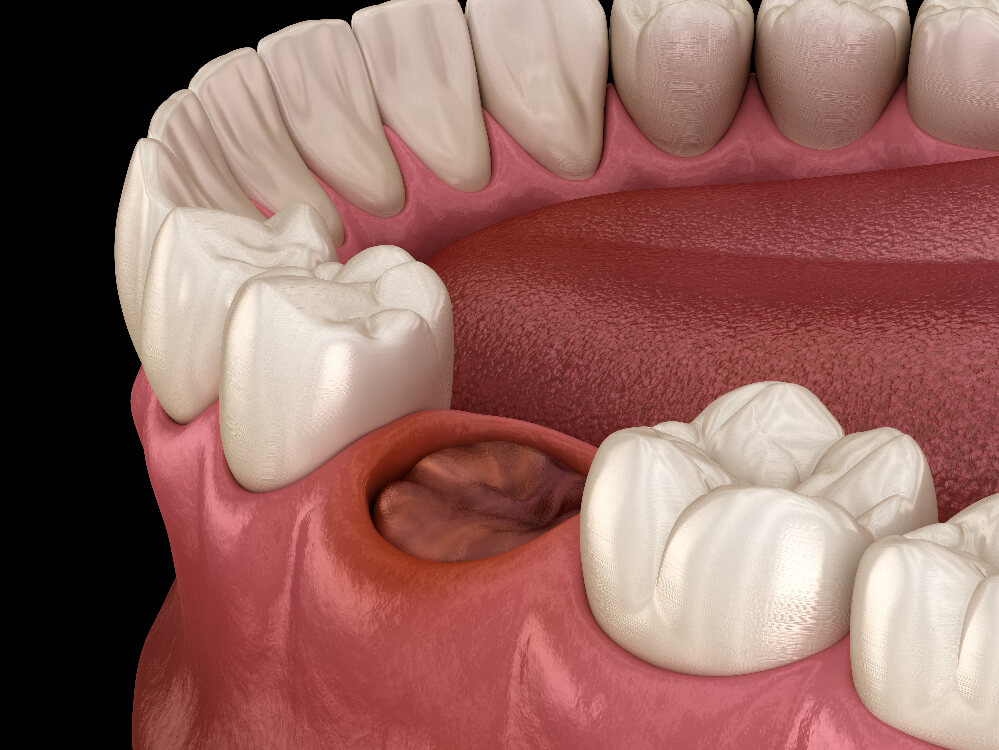
Dry Socket: If you experience intense pain a few days after extraction, it could be a dry socket, which requires immediate dental care.
These complications are rare, but recognizing them early can prevent further issues.
Alternatives to Tooth Removal
In some cases, there may be alternatives to removing an infected tooth, depending on the extent of the infection and damage:
Root Canal Therapy: This procedure removes the infected tissue inside the tooth, potentially saving it.
Antibiotics: In minor infections, antibiotics can sometimes clear up the infection without the need for extraction.
Dental Crowns: If damage is extensive but the tooth root is intact, a crown can protect and preserve the tooth.
Your dentist will discuss the best options for treating your infection and saving your tooth if possible.
Conclusion
An infected tooth is a serious condition that requires prompt attention. If you’re experiencing pain, swelling, or other symptoms of an infection, consult a dentist to determine the best treatment. While tooth removal may sound intimidating, it’s often the safest solution to prevent further complications. With proper aftercare, most people recover quickly and experience relief from the pain and discomfort of infection.
FAQs
Why might I need a tooth removal?
Tooth removal is commonly required due to severe decay, infection, damage that cannot be repaired, or overcrowding. Wisdom teeth, which may not have enough room to emerge, often need to be removed as well.
How is tooth removal performed?
The procedure is typically performed by a dentist or oral surgeon. For simple extractions, the tooth is loosened and pulled out. For more complex cases (e.g., impacted teeth), surgery may be required to remove the tooth in pieces.
What is the recovery time after a tooth removal?
Recovery usually takes about 1 to 2 weeks. Swelling and discomfort are common initially but can be managed with prescribed pain relievers and ice packs. It’s important to follow post-operative care instructions to ensure proper healing.
What are the risks associated with tooth removal?
Although generally safe, risks include infection, dry socket (when the blood clot dislodges from the extraction site), and damage to nearby teeth or nerves. These risks are low, but it’s essential to follow care instructions to minimize complications
Can I eat normally after a tooth removal?
For the first few days, it’s advisable to eat soft foods and avoid chewing near the extraction site